Read the latest newsletter from the Community Health Clinic
2025 Shop House Auction - Phone Bids Now Open!
A New Shop House Building will be auctioned off via phone bid to benefit the Community Health Clinic. Phone bids are now open! The 48’ x 72’ shop will be built in just a few days by local construction crews who are donating their time. The shop must be built in a 25 mile radius of Honeyville, IN.
You can call and leave a bid anytime. Starting bid is $120,000. You can call and leave a bid anytime, where we keep high bid on voicemail 574-642-0444, until April 8, 2025 where we will FINALIZE OVER THE PHONE AT (574) 642-0444 AT 4:00 PM.
Successful bidder can work with the contractor to customize the shop to meet their needs. All proceeds go toward The Community Health Clinic. This building is built by our local construction crews who are donating their time. For questions about the building project, call Gerald Bontrager from Riverland Construction at 260-761-2162. Changes to the specs can be done, but with extra cost.
Reflecting on a Successful Dutch Dinner: Thank You for Your Support!
What an incredible night! The Community Health Clinic's annual Dutch Dinner held Saturday, November 9, 2024, was a beautiful celebration of community, commitment, and care—and we want to take a moment to express our deepest gratitude to everyone who attended and supported the event.
Thanks to the generosity of so many, this year’s dinner was a huge success. The evening was made possible by over 100 volunteers who dedicated their time and energy to plan, prepare, and serve the meal. From the food to the youth choir’s singing, every detail was a result of the hard work and care from individuals who are passionate about our mission and the families we serve.
A Heartfelt Thank You to All Who Made It Possible
We want to offer a special thanks to several key contributors whose support went above and beyond:
The Dutch Dinner Planning Committee: Their dedication and vision helped bring this event to life, creating an unforgettable experience for all involved.
CHC Contact Couple Volunteers: These volunteers worked tirelessly to prepare and serve the meal, ensuring every guest felt welcome and cared for.
Organic Valley (Middlebury): Thank you for providing the delicious appetizers that kicked off the evening!
Miller Poultry (Orland): Your generous donation of chicken made for a hearty and memorable meal.
Patient Family Members: We are deeply grateful to the families who shared their personal stories, offering a heartfelt reminder of the impact our work has on the lives of those we serve.
The Singers: Their beautiful vocal performances added a special touch to the evening’s atmosphere.
Heritage Unlimited: Thank you for crafting the beautiful plaques that recognized our supporters and volunteers.
Special Friends of CHC: Thank you for your craftsmanship of the live auction items.
Coming Together for a Greater Cause
We also want to extend our gratitude to all the volunteers, sponsors (see below), new friends, and familiar faces who came out to support the event. Your involvement in this evening—whether through donations, time, or simply showing up—plays an essential role in helping us continue our mission: to ensure that all children can grow up healthy, happy, and productive.
The Dutch Dinner is more than just a fundraising event—it’s a testament to the strength of our community and the power of working together to make a difference. The funds raised will help sustain the life-changing work of the Community Health Clinic, and we couldn’t do it without you.
Dr. Zineb Ammous, Clinical & Biochemical Geneticist, and the CHC’s Medical Director, gave the evening’s featured presentation titled, “The Cycle of Learning in the Search for a Cure.”
Propionic Acidemia (PA) is a rare genetic disorder affecting Plain and non-Plain families. Affected individuals cannot break down parts of protein and some types of fats due to a non-functioning enzyme resulting in the buildup of harmful substances. These substances can damage vital organs including the heart and the brain. Dr. Zineb Ammous, The Community Health Clinic’s Medical Director, and patient family members shared stories of what they are learning in their work together to ensure earlier diagnoses and better treatments on the journey in search of a cure for PA.
Looking Forward to the Future
As we reflect on the success of this year’s Dutch Dinner, we are filled with gratitude and optimism for the future. Thanks to the support of people like you, we’re able to continue providing essential healthcare services to families in need. Together, we’re making a lasting impact on the health and well-being of our community, and we couldn’t be more excited for what lies ahead.
Thank you once again for your unwavering commitment to our mission. We look forward to seeing you at future events and continuing to work together to ensure a healthy future for all children.
With heartfelt thanks,
The Community Health Clinic Team
Stay tuned for updates on upcoming events and ways you can continue to get involved! Don’t forget to follow us on Facebook and Instagram for the latest news.
2024 PLATINUM SPONSORS
GOLD SPONSORS:
ANONYMOUS
SILVER SPONSORS:
ANONYMOUS
PLAIN CHURCH GROUP MINISTRY
BRONZE SPONSORS:
Anonymous (5)
A & M Woodworking
BioMarin
Community Foundation of Elkhart County
D. Gaeddert Real Estate
Family Value Flooring, Inc
Forest River
Happy Stork Midwifery
Heartland Bike Shop
KC Innovations, LLC
L & M AG
LaVerne's Repair Inc.
Legacy Home Furniture
Peaceful Beginnings Midwifery
Rhythms of Grace Midwifery Care
Sunrise Seeds Plus, LLC
The Birth Center at New Song
Townline Furniture LLC
Troyer’s Masonry and Repair LLC
Bringing Hope to LGMD families
The CHC Team recently attended training in Richmond to expand LGMD research efforts.
The world’s highest concentration of individuals with LGMD R1/2A (calpainopathy) hail from Indiana’s Adams and Jay Counties, where at least 150 affected live within a 20-mile radius and more that one in 400 babies are born with the disease. The Community Health Clinic (CHC) is a medical home for these patients, providing them with affordable genetic testing, counseling, and medical care.
Based on this extensive clinical experience and the trust on which it is founded, the CHC recently became a site for the GRASP study.
Rapid advances in genetic therapy for Duchenne muscular dystrophy and LGMD R4/2E have set the stage for LGMD R1/2A, but therapeutic development has outpaced clinical trial preparedness. Calpainopathy is the most common form of LGMD, accounting for 30% of LGMD worldwide, but there are currently no approved therapies to alter the natural course of the disease.
Calpainopathy should be amenable to several emerging therapeutic approaches, including gene replacement, gene editing, and myostatin inhibition. Therapeutic development depends critically on rigorous natural history data as the basis for the design of clinical trials. It is vital to identify the health outcomes that are the most meaningful to patients and their relationship to measurable biomarkers. These form the indispensable foundation for enabling high-quality and successful clinical trials.
At the CHC, we’re honored to participate in this process and inspired by the opportunity to support clinical trials that bring new hope to the families we serve.
This article was written by Zineb Ammous, MD, FACMG, CLinical and Biochemical Genetists Medical Director, The Community Health Clinic and was originally published in the LGMD News Magazine Summer 2024 Vol. 4 / Issue 3.
About The Community Health Clinic
The Community Health Clinic (CHC) is a 501(c)(3) non-profit healthcare facility located in Shipshewana, Indiana, that provides specialized genetics care consistent with Amish and Mennonite (Plain) values. The CHC provides clinical genetic services to all individuals, regardless of religion, race, or age. Over the past 11 years, the CHC has grown into a successful rural genetics clinic and a thriving clinical research center. The CHC currently serves 1,500-2000 individuals per year with special healthcare needs related to genetic conditions. As a medical home for patients and families with complex genetic conditions, our team of health professionals work hard to help patients and their families get needed medical care for the best possible health outcomes.
Save the Date - Dutch Dinner 2024
The 13th Annual Dutch Dinner to benefit The Community Health Clinic will be held on Saturday, November 9, 2024 at the Sammlung Platz Event Center in Nappanee, Indiana.
The CHC’s Annual Dutch Dinner is a fun-filled evening where guests hear personal reflections about the Community Health Clinic’s local, state, and global impact, enjoy an authentic, family-style Amish dinner, and have the opportunity to ensure the clinic continues to help improve the lives of those affected by rare disorders.
The annual Dutch Dinner began 13 years ago to build awareness about the Community Health Clinic and raise support for its mission. The aim is for area business professionals, healthcare providers, and the general community to become acquainted with the value of the clinic’s work.
To find out more, to purchase a ticket or for sponsorship opportunities, Call 260-593-0108 ext 100, email development@indianachc.org, or visit indianachc.org/dutch-dinner-2024
Thank you for your consideration of support. We look forward to seeing you at the Dutch Dinner!
Lactation & Feeding Support with Michiana Lactation
The Community Health Clinic is excited to announce a new partnership with Michiana Lactation to offer lactation & feeding support at no cost for our patients.
Lauren Dill is an International Board Certified Lactation Consultant (IBCLC) supporting families in their infant feeding journeys. Often feeding our babies looks different than what we’d imagine, and Lauren is here to walk with families through their options and support them in each of their unique paths.
Lauren’s journey to become a lactation consultant began because of the challenges she met with her own children, each with their own special circumstances. She has worked in a number of different settings, including the Branch – Hillsdale – St. Joseph County WIC clinic, a dental office, midwifery practice, and owning her own private practice here in Shipshewana. She has continued her education and expanded her skill set in such areas as postpartum mood disorders, tethered oral tissues, airway development, oral habilitation, and oral reflex testing. She desires to inform families of their options, give them practical skills to help their babies thrive, and support them in whatever best decisions they make for their families.
Why would you see a lactation consultant?
You are expecting & wish to breastfeed your baby.
Prenatal visits are especially beneficial for first time parents or families who’ve struggled with breastfeeding in the past. A prenatal visit will include a medical history, identifying and underlying issues that can make breastfeeding difficult, pregnancy health history, discussing pregnancy complications that can sometimes pose challenges to successful feeding, a short presentation reviewing realistic expectations for breastfeeding in the early postpartum period, and plenty of time for questions and discussion surrounding each family’s unique needs.
Mom is having pain with feeding.
While nipple soreness during feeds and some engorgement is normal during the earliest stages of breastfeeding, pain is not. Moms should not have to grit their teeth, curl their toes, or swear under their breath when they latch their baby, nor should they be repeatedly fighting off clogged milk ducts and mastitis. Typically pain is something that can be improved with deeper latch or improved oral motor function during feeding. This often means positioning changes, breast shaping, gentle massage, and some functional exercises to be done at home are the keys to improvement.
Baby is unable to latch or stay latched.
Babies are designed to feed. Lactation consultants recognize feeding as the very first milestone after delivery, and an inability to latch means there is something off. Sometimes that means Baby needs a little extra stimulation during a feed, and sometimes it means there is some weakness, tension, or dysfunction that can be worked out. Lactation consultants can help with this regardless of if a baby is breast or bottle fed.
Baby is not gaining weight well or mom suspects she has low milk supply.
While there are sometimes medical reasons why infants are not gaining weight well, more often it is a situation of poor milk transfer (getting milk from mom to baby) or low milk supply. In either situation, a lactation consultant can work with families to provide them tools and options to optimize milk intake for Baby.
You are transitioning feeding methods.
This can mean moving from tube, bottle, breast, or shield, to anything else. Infants are creatures of habit, and the transition can be challenging and sometimes time consuming. Lactation consultants can make the transition feel more fluid, comfortable, and ultimately successful. We are trained to not only make it physically possible, but also help carry some of the emotional burden as well.
Your feeding plan has changed.
Often postpartum doesn’t look like we’d envisioned. Sometimes instead of nursing our babies, we must pump or offer formula. Sometimes mothers must stop lactation sooner than they’d planned. Transitioning from breastfeeding to pumping or formula feeding can mean our bodies are going through changes they’re not ready for. A lactation consultant can provide the tools needed to make those changes more comfortable and achievable.
Your baby is fussy, gassy, or difficult to settle.
Sometimes babies who are struggling with gas, colic, or reflux are actually having feeding-related challenges. A lactation consultant can assess function, educate on dietary changes, and offer tools to help settle these babies, making it possible for families to really enjoy their children during this stage.
You just need encouragement.
Often a lactation consult really ends up being a reminder that families really are thriving. Some parents just flourish with the extra set of eyes on their babies and words of encouragement. A quick weight check, latch assessment, and discussion on what to expect moving forward can help achieve that.
Lauren is at the Community Health Clinic on Mondays and offers office visits to our community at no out of pocket cost. To schedule a visit with Lauren, call Michiana Lactation at 260.207.4020, and let them know you are a patient at the Community Health Clinic when you call.
All About Hypertrophic Cardiomyopathy (HCM)
FAMILIAL HYPERTROPHIC CARDIOMYOPATHY, TYPE 4 (HCM4)
What is Hypertrophic Cardiomyopathy?
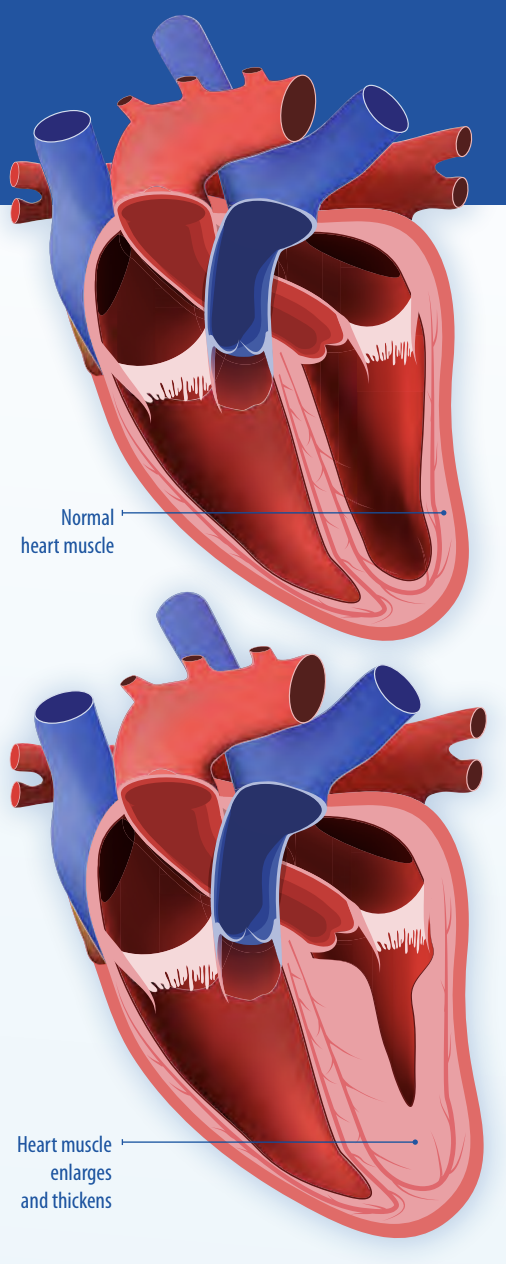
Hypertrophic cardiomyopathy (HCM) is a heart condition characterized by thickening (hypertrophy) of the heart (cardiac) muscle. Thickening usually occurs in the muscular wall that separates the lower left chamber of the heart (the left ventricle) from the lower right chamber (the right ventricle). This can lead to the heart having difficulty pumping blood to the rest of the body and also to abnormal heart rhythms (arrhythmia).
How common is Hypertrophic Cardiomyopathy (HCM)?
HCM is the most common genetic heart disease in the United States and affects at least 1 in 500 people. MYBPC3 gene mutations cause up to 30% of genetic HCM. When HCM is caused by a MYBPC3 gene mutation, it is known as HCM type 4 (HCM4).
What causes HCM4?
A mutation or DNA change in a gene called MYBPC3 causes an abnormally short or altered cardiac MYBP-C protein that does not work as well. This protein plays an important role in the structure of the heart muscle, so when a person inherits one mutated copy of the MYBCP3 gene, he or she is at risk to develop HCM4.
How is HCM4 inherited?
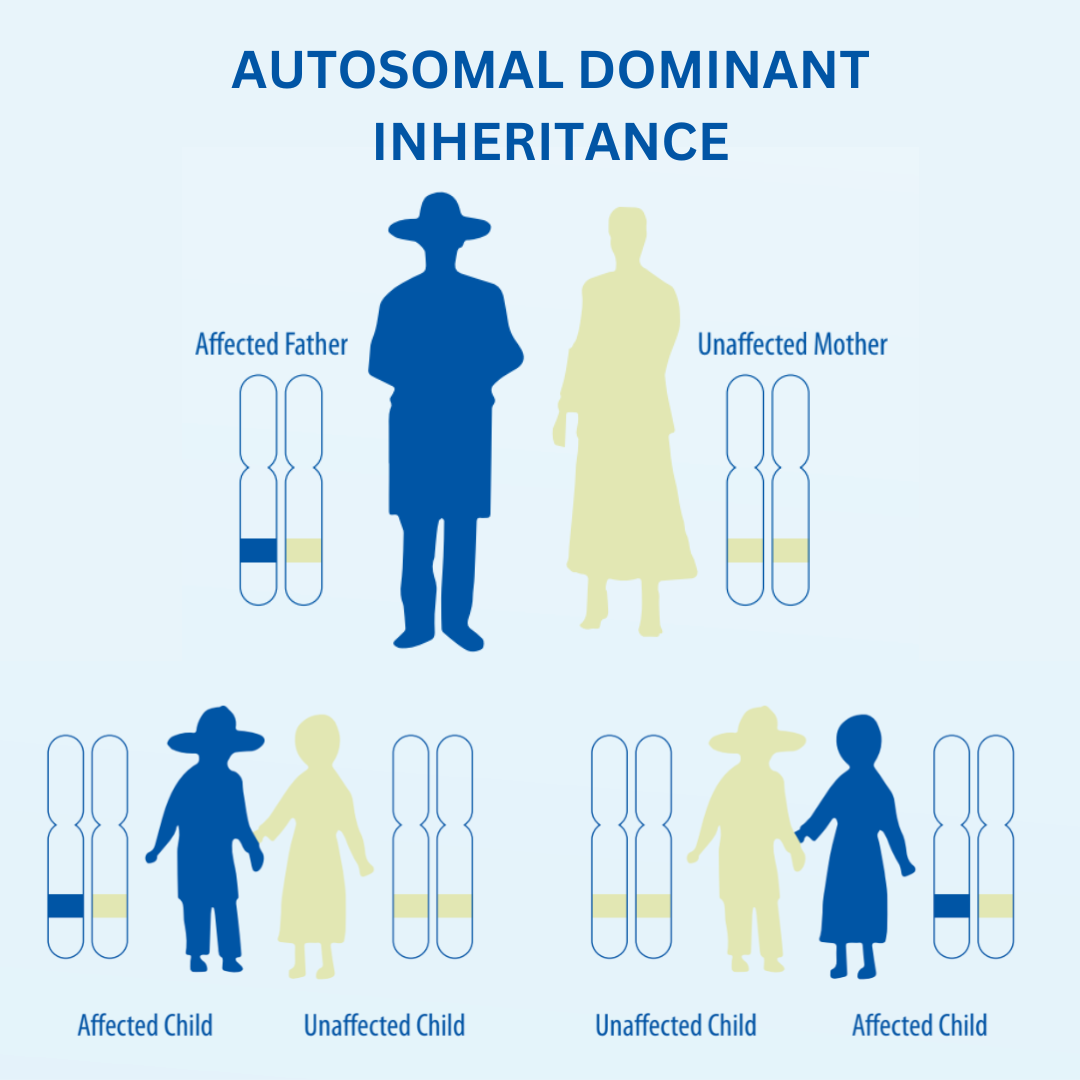
HCM4 is inherited in an autosomal dominant manner. This means that one mutation is needed in one of the two copies of the MYBPC3 gene for a person to be at risk to develop HCM4. A person who has a mutation in one copy of the MYBPC3 gene has a 50% chance to pass that mutation on to any of their children (regardless of whether they are boys or girls or whether the mutation is in Mom or Dad). The siblings of a person with HCM4 also have a 50% chance to have the MYBPC3 mutation.
When two people who both have one MYBCP3 gene mutation have children together, there is a 25% chance with each pregnancy for a child to inherit two MYBCP3 gene mutations (one from each parent). This leads to no working copies of the MYBCP3 gene and very little functioning MYBP-C protein in the heart.
Most babies develop very severe heart disease at a young age (within a few months to a few years after birth). Therefore, we recommend that the spouse of anybody with a known MYBCP3 mutation get testing themselves (even if there is no known family history of heart problems or a MYBCP3 mutation).
What is the treatment for HCM4?
There are no therapies that “cure” HCM4 but there are many treatments that improve symptoms and decrease the risk of complications. These include different types of medications, procedures to correct abnormal heart rhythms, and even heart transplant in very advanced cases. The earlier treatment can be started the better the outcome.
Symptoms of HCM4 are monitored using an echocardiogram (ECHO), which is an ultrasound of the heart. An EKG can also be done to look at the heart’s rhythm.
Who should have genetic testing for HCM4?
Genetic testing is performed to see whether a person has a mutated copy of the MYBCP3 gene. Anyone with a personal and/or family history of the following should consider genetic testing:
Hypertrophic cardiomyopathy (HCM) diagnosed on echocardiogram
Previous genetic testing that is positive for a mutation in the MYBCP3 gene
Heart disease and/or sudden death (especially at a young age –less than 50 years old)
In the setting of a known family history of a MYBCP3 gene mutation, we recommend testing for at-risk relatives by the age of 10-12 years old since this is the age at which cardiac screenings (echocardiogram, EKG) would begin for individuals who have a positive genetic test.
Spring / Summer 2024 CHC Newsletter
What is Occupational Therapy?
This April, the Community Health Clinic (CHC) l is celebrating Occupational Therapy Month!
We're grateful to have Dr. Erin Kline on our team to offer occupational therapy services for children with developmental delays. Her dedication to helping patients live life to the fullest is an inspiration! In this blog post, we’ll explain occupational therapy and the role it could play in your child's life.
What Is Occupational Therapy?
In general, occupational therapy (OT) helps people participate in meaningful activities, which are what we call "occupations." For a child, it includes activities such as feeding themselves, dressing themselves, playing with others, and learning at school. However, some children have challenges with these occupations for various reasons which requires the service of OT.
To address these delays, OT works on improving their performance in areas such as fine motors skills, visual perceptual skills, coordination, strength, sensory processing, and social skills.
What Can I Expect During an Occupational Therapy Appointment at the CHC?
During your first visit, the OT will evaluate your child through standardized assessments, observation, and discussion to determine the child's greatest needs. Goals are then created in collaboration with the family. The therapist will determine how often the child needs to be seen for therapy and provide the family with activities to do at home to help the child grow to their full potential!
Who Benefits from Occupational Therapy?
In general, OTs work with children who have developmental delays in fine motor, self-care skills, and difficulty with sensory processing.
Common diagnoses include:
Down Syndrome
Cerebral Palsy
ADHD
Autism Spectrum Disorder
Sensory Processing Disorder
Muscular Dystrophy
Genetic Disorders
How to Receive Occupational Therapy Services
First, contact your doctor to discuss your child's need for therapy services to receive a referral. If you would like services at the CHC, have them send it to us! We will then call to schedule for an initial evaluation.
*This program is currently not accepting Medicaid and is self-pay only.
Special Thanks to Our Building Campaign Contributors
We are most grateful for and humbled by the many hands that came together contributing the funds, labor, materials, and expertise that helped make this $4.06 million project possible. With thoughtful planning and your generous support, we were fortunate to move into the first clinic building of our own, on time, and on budget.
Now in our 11th year of service, and mostly settled in the new facility, we have already been able to meaningfully grow our clinical services, education programs, and patient-centered research initiatives. None of this work is done alone. Without the collaboration of our patient families, the communities we serve, and a growing number of medical and research partners, this work would not be possible.
Thank you again to the many friends who share our mission & vision and work together with us to advance medical knowledge and improve the quality of life for all those affected by rare disorders.
The Community Health Clinic's Special Edition Newsletter
Community Health Clinic’s Spring 2023 Newsletter
The latest Community Health Clinic Newsletter is here!
The Key to Optimal Health
by Marissa Testa, MS RDN LD
“Does that have seed oils in it?”
“Is that gluten free?”
“I only eat whole foods.”
The list could go on and on. However, at the root of all the statements and questions above, is the search for “optimal” health. This is not something new to 2023. In the 80’s, low fat food took center stage. The 1990’s came and went with Adkins diet. In the 2000’s, access to supplements became all the more widespread as did many new strategic ways to eat through the availability of new foods and supplements via the internet, new products and next day shipping.
Has any of this made a difference?
There is a difference in how we eat now versus how we used to eat.
For one, Americans love pastries and breads, which makes up the majority of most people’s diets. Our butter intake, while decreasing, has been replaced with vegetable sourced oils. Fruit and veggie intakes have decreased when compared to the 1970’s with only 10% of the American public eating the recommended servings of fruits and vegetables daily. Additionally, most Americans report they seek a healthy diet, while over half of the report that they should do better most days of the week.
These data trends are concerning for typical Americans. When you consider children with special health care needs, the prosect of pursing a heathy diet seems grim and overwhelming to choose the “right foods” to feed a growing child, much less one with special needs, texture aversions and swallowing difficulties.
On average, children with special healthcare needs are nearly twice as likely to experience food insecurities and malnutrition than a child with less healthcare needs.
So, what can we do to improve our own eating habits and those of these children in our care?
Here are 2 tips to better your or your child’s health without jumping to extremes:
Drink some water.
Sounds simple. However, most people do not drink enough leading to a chronic state of dehydration and even constipation. This can then affect appetite and overall quality of diet. The Centers for Disease Control and Preventions estimates 43% of Americans drink less than 4 cups a day, or half of the recommended 8 cups of water recommended per day for adults.
To drink more water, start by noticing how much plain water you drink in a day. The next day, try increasing your previous days amount by one cup and do this for a few days before increasing again. By increasing your or your child’s water intake slowly, you can avoid the constant urge to use the restroom and make the habit stick.
Eat some fruit. And some vegetables.
Again, easy right? The guidelines for Americans emphasizes fruits and veggies should make up half of a person’s plate each meal with a goal of 5 servings per day. However, the reality is, most people are not to this goal.
To work towards it, consider how many servings of fruits and vegetables you consume in a day. While having it in your refrigerator is wonderful, it doesn’t count unless it makes it in your body. Start by looking at the produce already in your home.
Does it go bad? Is it too hard to grab quickly? Prepping food by cutting it up before you need it can help make fruits and vegetables easier to eat. Also, by looking at your daily habits, you can make small changes like adding extra vegetables to your soups, more steamed broccoli to Chinese carryout or bananas to your oatmeal to work towards the 5-a-day habit.
For kids, exposure and modeling are key. Kids watching adults eat healthy are more likely to eat fruits and vegetables themselves. Children also may need to try a new food up to 10-15 times before it is accepted- if they have developmental delays this can be up to 30 times of seeing a food before it even makes it into their mouth!
If wasting food is a concern while trying to also expose your child to new foods, try freezing scraps and using them in smoothies as a new way to encourage acceptance with foods in a new texture! Sometimes offering foods warm or frozen (as long as they aren’t a choking hazard) can also help kids be more willing to try a new fruit or vegetable.
Change Towards a Healthy Diet Takes Effort
Overall, as with anything, change towards a healthy diet takes effort (as well as water and fruits and veggies!) Making a plan and taking a small first step can help you build momentum to make big live changes to improve your overall health.
A registered dietitian is a great resource to help you and are now more available than ever through groceries stores, telehealth and your local Community Health Clinic. They can assist with specialized diets for specific conditions to help you or your child work towards a healthier diet step by step.
Marissa Testa, MS RDN LD, is a remote metabolic dietitian at the Community Health Clinic.
Her passion is enteral nutrition, home-blended formulas and patient education making every family feel that they can feed and grow their children regardless of medical diagnosis.
Marissa lives in Columbus, Ohio with her husband Michael and also homeschools her three children. She will very willingly accept any recipes you are willing to share.
New Clinic Building Construction Spring Update
With the shell of the building largely completed last fall, much progress has been made on the interior of the Community Health Clinic’s new facility over the winter.
Mechanicals, sheet rock, flooring, and trim carpentry are largely complete on the first and second floors. On the lower-level walkout basement, interior work is underway on the Community Education Room, demonstration kitchen for our dieticians’ programs, restrooms, and the staff locker room. Less than half of the full basement will be finished, the balance will be reserved for future needs in the years to come.
Work on the interior of the building should be completed by early summer and will leave us in good shape to complete paving, landscaping, furnish the spaces, and move in before fall.
We look forward to welcoming the community to our Open House & 10th Anniversary on September 9, 2023. Save the date, more details to follow.
Second floor looking south – March 3, 2023
Community Education Room – March 3, 2023
Special thanks go to Freedom Builders, the general contractor, and the subcontractors on this project. We appreciate their expertise and quality work! We are also most grateful for those who have contributed labor and materials to help keep the project on schedule and on budget.
Many hands have come together to make the first facility of our own possible. We’d like to again express our gratitude to all those who contributed to the capital campaign.
If you have any questions about the campaign, or might like to help, please contact Blake Andres, Director of Development and Planning at bandres@indianachc.org or office: 260-593-0108, mobile: 440-463-9912.
2023 Work Shop - Phone Bids Now Open!
A New Shop Building will be auctioned off via phone bid to benefit the Community Health Clinic. Phone bids are now open! The 44’ x 64’ shop will be built in 2 days by local construction crews. The shop must be built in a 25 mile radius of Honeyville, IN.
You can call and leave a bid anytime. Starting bid is $100,000. The high bid is on voicemail at 574-642-0444, until April 12, 2023 where we will Finalize over the Phone at 574-642-0444 at 4:00 pm.
Successful bidder can work with the contractor to customize the shop to meet their needs. For questions on this building project, Call Marlin Bontrager at 574-825-1075.
Community Health Clinic’s Winter 2022 Newsletter
The latest Community Health Clinic Newsletter is here!
New Clinic Building Construction Update
Progress on the CHC’s new facility is moving forward according to schedule. After the groundbreaking in May, foundation work commenced in June and framing of the two-story building began in July. As of November 1, the shell of the building is nearly complete, and work has begun on the mechanical and electrical systems. Our goal is to have the facility completed in the summer of 2023 and be moved in by September - in time for our Community Health Clinic’s tenth anniversary.
The main floor of the new building features an increased number of patient care rooms to meet the needs of a growing community. These rooms will be significantly larger, providing increased comfort for patient families with complex medical needs. The building will support and grow existing partnerships and new collaborations providing expanded services including sub-specialty clinics, such as hemophilia, neurology, cardiology, and others.
Our new clinic will have dedicated rooms for genetic counseling, dietary services for those with metabolic disorders, and spaces to host an increased number of patient-centered research studies. Our research focus is twofold: building enhanced understanding of the rare genetic disorders that affect our patient families, and leveraging that understanding to help develop new therapies and treatments. The facility will also have several meeting rooms to accommodate both small and larger groups. The walkout basement features a Community Room to host education events and disease-specific family gatherings. To date, we have not had those capabilities, having to borrow, or rent space to bring families together.
If you have any questions about the campaign, or would like to help in some way, please contact Blake Andres, Director of Development and Planning at bandres@indianachc.org or 260 593-0108.
The Community Health Clinic Doses First Patient in Phase 1 Trial of BBP-671, a Potential Treatment for Propionic Acidemia (PA)
TOPEKA, IN — The Community Health Clinic, a clinic which specializes in rare diseases, recently dosed the first propionic acidemia patient with an investigational new drug for Propionic Acidemia (PA) and Methylmalonic Acidemia (MMA). The patient was successfully dosed in the second part of BridgeBio Pharma, Inc.’s Phase 1, first in-human clinical trial of BBP-671 in patients with PA and MMA. BBP-671 is an investigational oral therapy being developed as a potential treatment for diseases in which coenzyme A (CoA) metabolism is deficient, including PA and MMA. It is intended to increase coenzyme A (CoA) levels by allosterically modulating pantothenate kinases, key enzymes in the CoA biosynthesis pathway.
The first patient dosed in this portion of the trial has PA. PA is a rare metabolic disorder caused by mutations in genes that impact the development of enzymes that participate in amino acid metabolism, leading to life-threatening metabolic decompensations, as well as long-term complications involving multiple organ systems, including the heart, pancreas, kidney, liver, and brain. The current standard of care for patients with PA or MMA includes dietary restrictions, supplementation, and sometimes liver and/or kidney transplantation but the need to develop a treatment for these conditions remains high due to the long-term and life-threatening impact of these diseases.
“Improving the care of individuals affected by propionic acidemia has been a passion of mine for the last 12 years. We hope that this trial will provide valuable data and ultimately lead to a meaningful therapy for individuals affected by PA and MMA who currently have no approved treatment options. Being part of this clinical trial is key to translating medical innovation to community health care”, said Zineb Ammous, MD, Medical Director of The Community Health Clinic.
“It’s truly exciting for our small clinic in Topeka, Indiana to play a part in this trial, which will have lasting effects for our community, and everyone affected by PA,” said Jared Beasley, R.N., Executive Director of The Community Health Clinic. “We’d like to thank the patient family, Parkview LaGrange Hospital and Topeka Pharmacy for their collaboration.”
More information about the trial can be found on clinicaltrials.gov.
###
About The Community Health Clinic The Community Health Clinic (CHC) is a 501(c)(3) non-profit healthcare facility located in Topeka, IN, that provides specialized genetics care consistent with Amish and Mennonite (Plain) values. Since their founding in 2008, The CHC has seen more than 4200 patients and 198 genetic disorders. For more information, please visit www.IndianaCHC.org.
Rhonda's Story
Rhonda Anderson is the Community Health Clinic’s (CHC) Nurse Practitioner. She has been with the clinic for one year now. At the clinic, Rhonda’s primary focus is to see patients on a follow-up basis for those with complex genetic disorders. She has also been involved in many of our outreach clinics including Berne and Paoli, Indiana.
Rhonda has also started seeing new patients for evaluations in collaboration with Nicole Bertsch, the clinic’s genetic counselor. Home visits for patients with multiple medical complexities is also a service that Rhonda provides for the CHC. Rhonda graduated with her Registered Nurse license in 2003 and then became a Nurse Practitioner in 2013 and started working in Complex Care Pediatrics. Rhonda has a strong clinical background professionally working with children with multiple complex medical conditions, but also personally, as she is the mother of a special needs child herself.
Rhonda has three beautiful daughters, Abby, Kylie, and Katie. Her youngest daughter, Katie, experienced many complicated medical issues starting at a young age which included failure to thrive requiring a gastronomy tube, a congenital heart defect requiring open heart surgery, recurrent illnesses, and significant developmental delays.
Dr. Ammous Zineb (Dr. Z) and Rhonda at the 2022 American College of Medical Genetics Meeting
Katie has multiple body systems affected and trying to find an answer to what was wrong with her was long and difficult. Katie had her first visit at the CHC in 2015 with Dr. Z to try and determine a cause for Katie’s multiple congenital anomalies. Genetic testing was performed which was normal. Katie was ultimately diagnosed with clinical CHARGE syndrome and autism. Katie now attends therapy weekly, receives gamma globulin infusions monthly, and follows with multiple specialists locally and at the CHARGE clinic at Cincinnati Children’s Hospital.
Rhonda understands the frustration parents experience when trying to find a diagnosis for their child. She also understands how difficult it can be to care for a child with multiple special needs. She has been to a variety of specialty services with Katie and is able to provide parents with feedback from a trusted resource. Rhonda was excited to join the CHC team and to be able to be an advocate for our families and help guide them in the right direction to doing what is best for their child.
Rhonda’s husband, Brad, is a retired Army veteran. Her daughter Abby just finished her freshman year at Indiana State University, Kylie is finishing her sophomore year at East Noble High School where she plays volleyball and softball. Katie has recently joined the Special Olympics track team.
In her spare time, Rhonda enjoys spending time with her husband and attending her girls’ events. Rhonda is also the high school volleyball booster coordinator, where she helps plan fundraising events, team dinners, and camps.
See More About Our Staff or Read Patient Stories.
CHC Begins Construction on New Building
The Community Health Clinic (CHC), a nonprofit healthcare facility that focuses on research and specialized care for individuals with rare genetic conditions, has begun construction on a new 15,000 square-foot facility on ten acres of land in North Shipshewana, Indiana.
The new building will allow the CHC to continue patient care, support program development, and improve the quality of life for a growing population of families affected by rare disorders. It will include an increased number of patient care rooms, workplaces for visiting clinicians, meeting spaces, and a large community room for education and related family gatherings.
Why a New Building?
Since the opening of the Community Health Clinic, we have been careful stewards of community resources, doing our work in a modest rented space, less than 3,500 square feet in the basement of a small medical building in Topeka, Indiana.
THE NEW BUILDING WILL ALLOW THE CHC TO:
Improve the quality of life for families affected by rare disorders
Help to decrease the time from diagnosis to treatment
Help advance cures with the hope that one day, all children may grow up to enjoy healthy, happy, and productive lives